17.Birke J & Sims D. The insensitive foot. In: Hunt G & McPoil T (eds). Physical Therapy of the Foot and Ankle (2nd ed). Churchill Livingstone, 1995 pp 159-200.
18.Birke J, Cornwall M & Johnson M. Relationship between hallux limitus and ulceration of the great toe. J Ortho & Sports Phys Ther 1988; 10(5):172-76.
19.Bennett P, Stocks A & Whittam D. Analysis of risk factors for neuropathic foot ulceration in diabetes mellitus. J Amer Podiatric Med Assoc 1996; 86 (3):112-16.
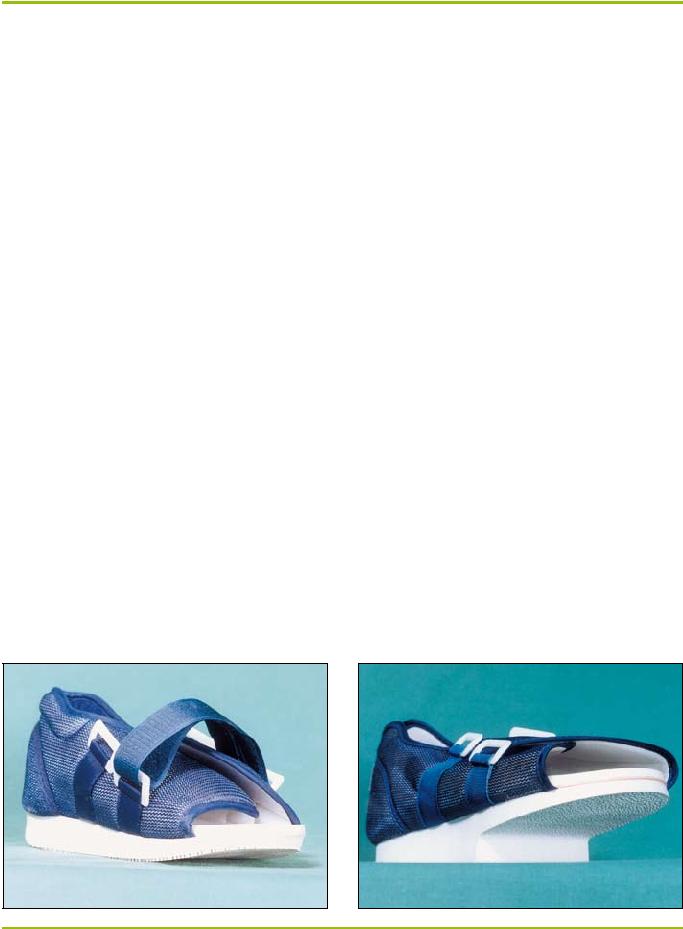
20.Coleman W & Plaia A. Soft moulded sandals for insensitive foot care. Clin Prosthetics & Orthotics 1988; 12(2):67-73.
21.Sarnow M, Eves A, Giurini J, Rosenblum B, Chrzan J & Habershaw G. In-shoe pressure measurements in diabetic patients with at-risk feet and in healthy subjects. Diabetes Care 1991; 17(9):1002-06.
22.Frykberg R, Lavery L, Pham H, Harvey C, Harkless L & Veves A. Role of neuropathy and high foot pressures in diabetic foot ulceration. Diabetes Care 1998; 21(10):1714-19.
23.Novick A, Stone J, Birke J, Brasseaux D, Broussard J, Hoard A & Hawkins E. Reduction of plantar pressure with the rigid relief orthosis. J Amer Podiatric Med Assoc 1993; 83(3):115-22.
24.Landsman A, Meaney D, Cargill R, Macarak E & Thibault L. High strain rate tissue deformation: a theory on the mechanical etiology of diabetic foot ulcerations. J Amer Podiatric Med Assoc 1995; 85(10):519-27.
25.Cochrane G. A Primer of Orthopaedic Biomechanics. New York: Churchill Livingstone, 1982.
26.Brill L, Cavanagh P, Doucette M & Ulbrecht J. Prevention, protection and recurrence reduction of diabetic neuropathic foot ulcers.(number 5 in a series). Treatment of Chronic Wounds (pamphlet).
27.Guzman B, Fisher G, Palladino S & Stavosky W. Pressure-removing strategies in neuropathic ulcer therapy. Cited in Clin Podiatric Med and Surg 1994; 11(2):339-53.
28.Murray H, Young M, Hollis S & Boulton A. The association between callus formation, high pressures and neuropathy in diabetic foot ulceration. Dia- betic Med 1996; 13:979-82.
29.Saye D. The foot: ulcer and toenail debridement and pressure-relief padding. Ostomy/Wound Management 1994; 40(6):14-25.
30.Armstrong D, Liswood P & Todd W. Potential risks of accommodative padding in the treatment of neuropathic ulcerations. Ostomy/Wound Management 1995; 41(7):44-49.
31.Armstrong D & Athanasiou K. The edge effect: how and why wounds grow in size and depth. Clin Podiatric Med & Surg 1998; 15(1):105-08.
32.Chantelau E & Haage P. An audit of cushioned diabetic footwear: relation to patient compliance. Diabetes Med 1994; 11:114-16.
33.Soulier S, Godsey C, Asay E & Perrotta D. The prevention of plantar ulceration in the diabetic foot through the use of running shoes. Diabetes Educator 1987; 13(2):130-32.
34.Nawoczenski D, Birke J & Coleman W. Effect of rocker sole design on plantar forefoot pressures. J Amer Podiatric Med Assoc 1988; 78(9):455-60.
35.Schaff P & Cavanagh P. Shoes for the insensitive foot: the effect of a rocker bottom shoe modification on plantar pressure distribution. Foot and Ankle 1990; 11(3):129-40.
36.Fleischli J, Lavery L, Vela S, Ashry H & Lavery D. Comparison of strategies for reducing pressure at the site of neuropathic ulcers. J Amer Podiatric Med Assoc 1997; 87(10):466-72.
37.Chantelau E, Breuer U, Leisch A, Tanudjaja T & Reuter M. Outpatient treatment of unilateral diabetic foot ulcers with ‘half shoes’. Diabetic Med 1993; 10(11):267-70.
38.Needleman R. Successes and pitfalls in the healing of neuropathic forefoot ulcerations with the IPOS postoperative shoe. Foot and Ankle Inter 1997; 18(7):412-16.
39.Birke J, Novick A, Graham S, Coleman W & Brasseaux D. Methods of treating plantar ulcers. Physical Ther 1991; 71(2):116-22.
40.Petchell A, Keenan A & Landorf K. National clinical guidelines for podiatric foot orthoses. Aust J Podiatric Med 1998; 32(3):97-103.
41.Albert S & Rinoie C. Effect of custom orthotics on plantar pressure distri- bution in the pronated diabetic foot. Foot & Ankle 1994; 33(6):598-604.
42.Brodsky J, Kourosh S, Stills M & Mooney V. Objective evaluation of insert material for diabetic and athletic footwear. Foot and Ankle 1988; 9(3):111-16.
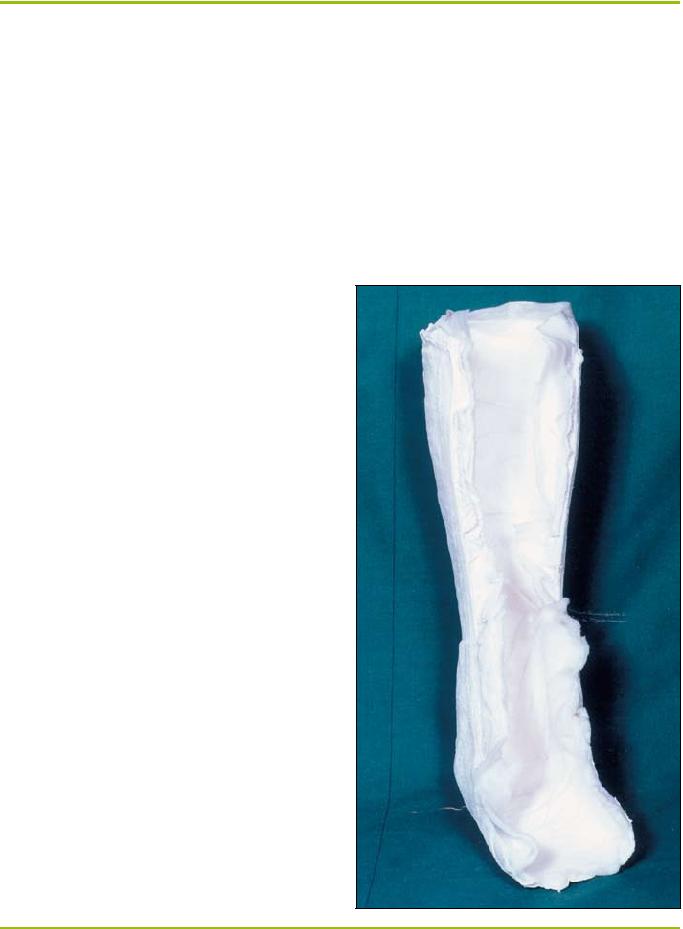
43.Burden C, Jones G, Jones R & Blandford R. Use of the ‘Scotchcast boot’ in treating diabetic foot ulcers. Brit Med J 1983; 28(6):1555-57.
44.Beiser I, Light M, Lynch T & Kanat I. The effect of various forms of immobilisation on plantar foot pressure. J Amer Podiatric Med Assoc 1991; 81(4):206-14.
45.Page S. ‘Neofract’ boots for diabetic neuropathic foot ulcers. J Brit Podiatric Med 1996; 51(2):19-23.
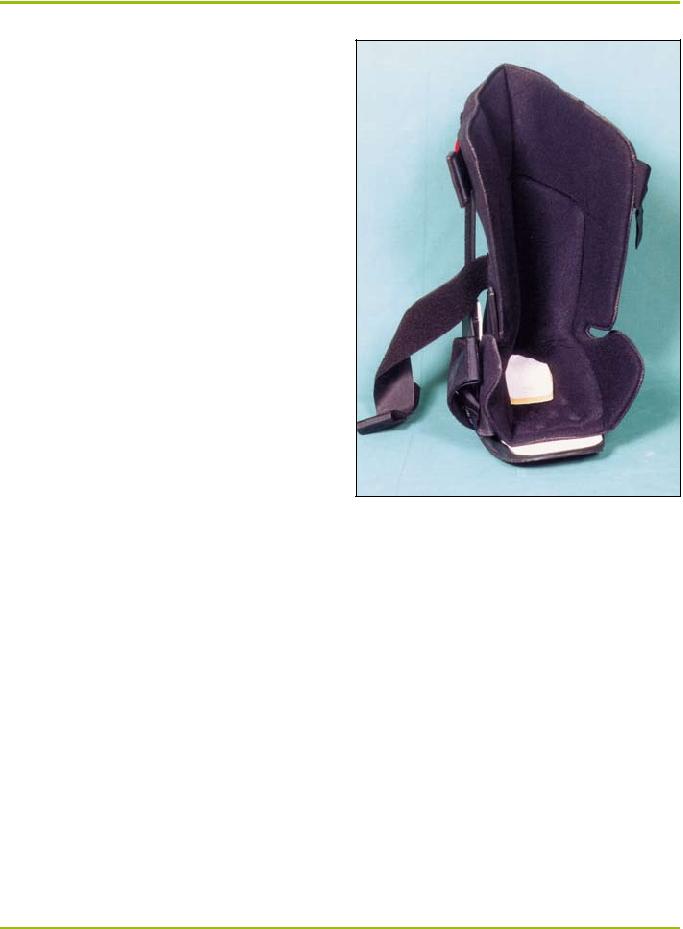
46.Sinacore D, Mueller M, Diamond J, Blair V, Drury D & Rose S. Diabetic plantar ulcers treated by total contact casting. Physical Ther 1987; 67 (10):1543-52.
47.Armstrong D & Lavery L. Evidence-based options for off-loading diabetic wounds. Clin Podiatric Med & Surg 1998; 15(1):95-104.
48.Ritz G, Rowland W & Rowland J. Use of the Cam walker in treating diabetic ulcers. J Amer Podiatric Med Assoc 1996; 86(6):253-56.
49.Nawoczenski D, Birke J, Graham S & Koziatek E. The neuropathic foot – a management scheme. Physical Ther 1989; 69(4):287-91.
50.Murray H, Veves A, Young M, Richie D & Boulton A. Role of experimental socks in the care of the high-risk diabetic foot. Diabetes Care 1993; 16 (8):1190-92.
51.Meuller M, Sinacore D, Hoogstrate S & Daly L. Hip and ankle walking strategies: effect on peak plantar pressures and implications for neuropathic ulceration. Arch Phys Med & Rehab 1994; 75(11):1196-1200.
52.Walker S. Sensory substitution in the diabetic neuropathic foot. J Amer Podiatric Med Assoc 1997; 87(7):338.
53.McGill M, Collins P, Bolton T & Yue D. Management of neuropathic
ulceration. J Wound Care 1996; 5(2):52-54.